Sarah A. Bajorek, PharmD, BCACP
Mithu Molla, MD, MBA
UC Davis Health
The University of California Davis Medical Center is a tertiary, 627-bed urban academic medical center that provides care to the Sacramento and northern California region. With a growing awareness of sentinel safety events related to medication errors, an internal assessment in 2015 gave us greater insight into opportunities for improvement around medication reconciliation practices. At that time, our small pharmacy medication reconciliation team (consisting of one pharmacist and two pharmacy technicians) was a consult-based service. The internal assessment, which included a time study, revealed pharmacy technicians spending an average of 45 minutes to complete a medication history, as compared to 10 minutes for medical residents and six minutes for attending physicians. The accuracy of the medication list inversely correlated with the time spent on gathering the history, and this lack of dedicated pharmacy technicians ultimately led to incomplete medication lists and greater medication errors. Additionally, there were problems obtaining refill histories from retail pharmacies in the community. Through an internal risk-reduction grant, four additional pharmacy technicians were added to our staff, as well as software that integrates pharmacy refill histories from pharmacies in the community.
Around the time that we were restructuring the med rec team, the Multi-center Medication Reconciliation Quality Improvement (MARQUIS 2) Study was recruiting organizations to participate in best practices approach to medication reconciliation. This was an opportunity for us to participate in a large multi-center collaborative of academic and non-academic hospitals focused on interventions that were shown to be effective in limiting medication errors. This was a mentored implementation program using structured quality improvement techniques. Through guidance and collaboration with other sites and leadership from MARQUIS, we created process maps, performed gap analysis, and created swim lane diagrams, revealing over 80 gaps in our medication history and reconciliation process from emergency department (ED) to hospital discharge. We then identified four areas of focus to improve our mediation reconciliation process:
- Leverage the four additional pharmacy technicians acquired through the internal grant
- Update our medication reconciliation policy to expand roles
- Train staff on best practices
- Leverage electronic medical records (EMRs) to streamline the process
To align our medication reconciliation efforts with institutional goals, we eliminated the consult-based service and assigned our medication history pharmacy technicians to the ED and three hospital units. The previous medication reconciliation policy restricted updating the medication list to providers and pharmacists. However, most of the medication history documentation was completed by pharmacy staff (technicians and students), nurses, and residents. They were able to add comments when medications needed to be removed from the medication list but were not allowed to remove them or touch the medication list. This inability to change the medication list and solely add comments created an inherently more passive role for our pharmacy staff, as those comments were frequently not acted on. Ultimately, inaccurate or expired medications persisted on the list. Therefore, we expanded the ability to remove erroneous medications from the list to add pharmacy technicians, nurses, and respiratory therapists (for respiratory medications). In addition, we updated the policy to reflect the intent of the medication list (i.e. what the patient is taking vs. what they were prescribed).
Lastly, we trained all pharmacy staff on medication history and reconciliation best practices (available through Society of Hospital Medicine). We utilized a combination of recorded lectures, competencies (as part of the on-boarding process for new hires, as well as annually), and shadowing to ensure pharmacy staff understood the process. In addition, we created standard phrases to communicate medication discrepancies to providers, such as “Not Current per patient due to X reason,” or “Non-formulary – please change to X medication,” or “Refill Required.” This helps guide providers to resolve these issues during both admission and discharge medication reconciliation. We also incorporated medication history and reconciliation best practices into new medical resident and attending EMR orientation, so they are familiar with the process and what is needed of them when they see the standard phrases communicating medication discrepancies.
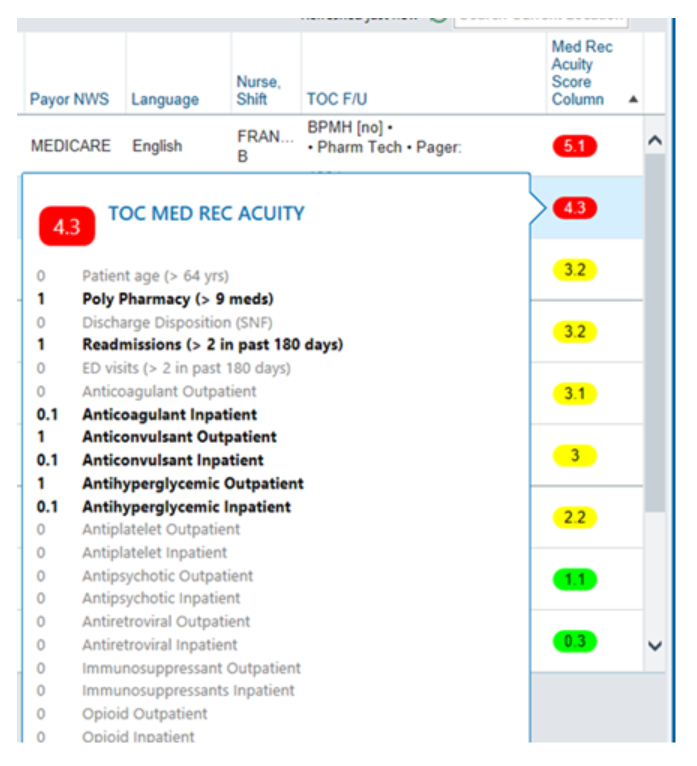
We worked with our EMR team to build enhancements to streamline the medication history and reconciliation process. For example, an automated risk scoring tool to risk stratify our patients helped us to quickly identify patients at highest risk for medication errors where we could target our resources. We previously risk stratified patients using a manual chart review process, which we found to be quite time consuming. The automated risk score assigns points based on discrete EMR data elements and helps us risk stratify patients into high, moderate, or low risk for medication-related errors.
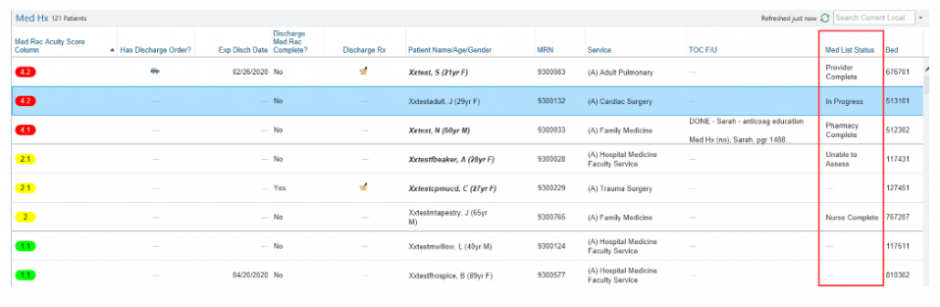
To prevent duplication of work and improve transparency, we built a patient list column that shows the status of the medication list.
All our interventions to improve medication histories and reconciliation were shown to be beneficial. Prior to our interventions, patients had five clinically significant discrepancies on their medication list. Post-implementation of the MARQUIS best practices bundle, we showed a 64% relative reduction in discrepancies as compared to control and 89% accuracy in the medication list as compared to 52% for control. We also saw improvements in our Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores for the Transitions of Care domain and Purpose of Medications question for our intervention units. Our four pharmacy technicians were only funded for two years with the internal grant, so we utilized the data to assess the financial impact of permanently hiring the four pharmacy technicians (net savings of $1.4 million) as compared to reverting to two pharmacy technicians (net savings $250,000). The return on investment made a compelling case to our executive suite to keep the pharmacy technicians on staff, and the four pharmacy technicians were permanently hired in July 2018.
On January 1, 2019, Senate Bill 1254 went into effect. This bill requires hospital pharmacy staff to obtain an accurate medication profile or list for each high-risk patient upon admission. To meet this requirement, we expanded medication histories hospital wide in January 2019. In addition, the hospital recognized all patients benefit from having a medication history done by pharmacy, regardless of their risk status. Therefore, one of the Department of Pharmacy’s goals for fiscal year ’20 is to have greater than 90% of medication histories completed by pharmacy for weekdays. We are currently meeting this goal.