On June 7, attendees at the Collaborative Healthcare Patient Safety Organization’s (CHPSO) Safe Table had a chance to hear from Barton Health about medication reconciliation and its approach to this difficult process.
Kaitlyn Clark, PharmD, and Cathy Deering, pharmacy med rec tech, stressed the importance of a partnership among providers, nursing, and pharmacy professionals. After Barton Health went live with the EPIC electronic medical record (EMR) system in 2012, efforts to refine the medication reconciliation (med rec) process began taking shape, requiring several adaptations. Entering med rec information once into the EMR’s designated area does NOT mean “job done” for the entirety of the patient’s hospitalization. This process is not a simple checklist item, but rather a continuous process from admission through discharge — even pre-admission and post-discharge when possible.
Background:
Perhaps the oldest focus of the patient safety movement — medication safety — is still one of the toughest to manage. Medication errors occur along a complex process chain: prescription orders, transcription, procuration, distribution, administration (including dosage, frequency, and route), omission, commission, timing, interaction, and the toughest of all — managing medications taken across health care settings and at home. To maximize safety across the continuum of care, the process of med rec was designed by patient safety experts and is required by regulatory and accreditation bodies to prevent errors and adverse events. However, conducting good med rec is as complex and challenging as any health care intervention can be.
Common difficulties that require more than simply listing medications include:
- Patient is not a good historian, and cannot articulate precise medication names, dosages, and/or frequencies of all meds taken at home
- Dosages are stated but turn out to be incorrect (i.e., mg vs. mcg, or once vs. twice daily)
- Two very similar medications are listed
Approach:
At Barton Health, cultivating a gold standard means following up on any of these or other inconsistencies or questions, and making certain that a med rec process entered into EPIC is marked “incomplete” if there are any such questions or potential discrepancies found on the first attempt. This is where the med rec tech comes in. Starting in 2016, a full-time med rec tech was added to the pharmacy staff, consistent with newer industry-wide recommendations for best outcomes. Prior to that, the pharmacist was often involved in supporting nursing staff in the med rec process but was unable to allocate enough time to address all the needs. Internal data suggested that approximately 50% of all med rec process entries were incomplete or incorrect in some way.
With this new approach, the full-time med rec tech:
- Meets with every patient
- Can spend more time with the patient or family when needed
- Uses various prompts to improve the completeness and accuracy of the information
- Can query outpatient clinics and pharmacies when necessary to clarify the current medications
The med rec tech role began with a focus on emergency room (ER) admissions and the plan was to station the tech in the ER. Several barriers with the availability of workstations and/or wheeled workstations resulted in a hybrid model. Now the med rec tech role is mobilized between the pharmacy, the ER, and the nursing units.
Initial Results and Refined Approach:
A significant decrease in medication reconciliation errors was achieved over the first three years with a dedicated pharmacy med rec tech. Then:
- In 2019, the pharmacy added efficiency and excellence by creating a Standard Operating Procedure and conducting cross-training sessions for nursing staff and outpatient clinic medical assistants (MAs).
- In 2020, the inclusion of an outpatient physician champion expanded the reach and scope of the collaboration with clinics, and a “tip sheet” for MAs was created.
- In 2021, COVID-19 communication challenges included navigating barriers with HEPA filters, negative pressure rooms, and more telephonic (rather than in-person) patient interviews.
- In 2022, the “Dr. First Med History” program was implemented, which clarifies questions for poor historians. This is a web-based technology that allows the hospital to query for prescriptions the patient has recently filled at community pharmacies. The current protocol now includes the ER intake staff running a report for the triage RN, and in the OR, the pre-op RN running a report prior to the pre-op call.
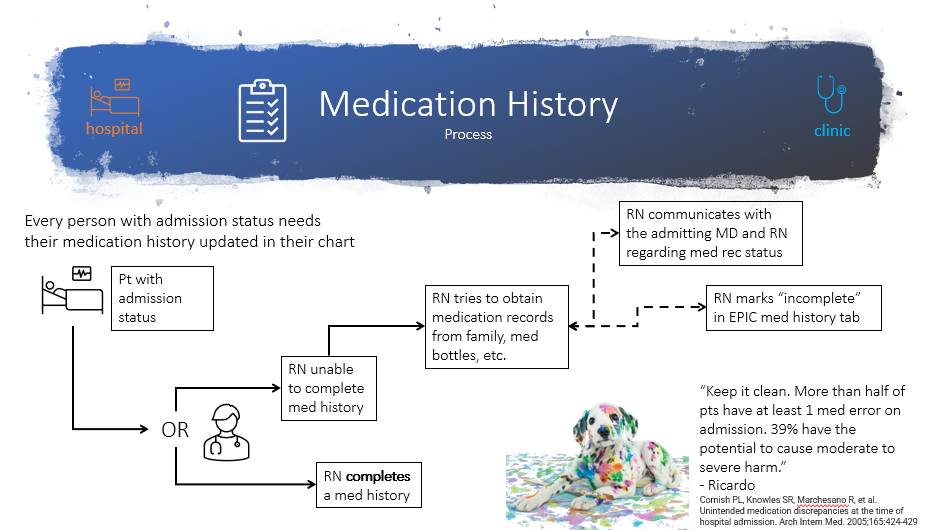
As of 2023, the education module has been refined with slides to address the med rec process and the correct entry points into the EMR. Collaborative training sessions are offered by pharmacy staff and include examples of potential errors that were averted, as well as tips and strategies that are continually learned along the way. The pharmacy team created an algorithm depicting the process that nursing staff follows to attempt completion of the initial medication reconciliation. The “incomplete” flag in the EMR helps the pharmacy med rec tech prioritize cases that need attention.
Next Steps:
Although the process is refined and successful, some medication reconciliation errors and resulting medication events do still occur and are highly correlated with the days and hours that the med rec tech is off work. Current plans to expand resources and improve program resilience include cross-training for other pharmacy technicians, and/or hiring additional staff dedicated to the med tech role so this service can be provided reliably seven days a week.
The presenters emphasized that their sites are focused on “cultivating” a gold standard, stressing that this is still a work in progress, but that collaboration among providers, nurses, and pharmacy staff provides the optimal multidisciplinary team for continuous quality improvement!
