A well-done root cause analysis (RCA) can save lives, especially when it is shared at a CHPSO Safe Table so that many hospitals can benefit. At a Safe Table in February, a CHPSO member shared a situation involving the death of a patient who was admitted for chest pain, abdominal pain, and alcohol withdrawal.
We are very fortunate that one of our member hospitals shared their experience with a patient who was well-known to them, a 65-year-old male with a history of chronic pancreatitis, hypertension, and seizures in the setting of alcohol withdrawal. After ruling out a coronary condition, abdominal aortic aneurysm, and dissection, clinicians continued treatment for alcohol withdrawal using the Clinical Institute Withdrawal Assessment (CIWA) for Alcohol.
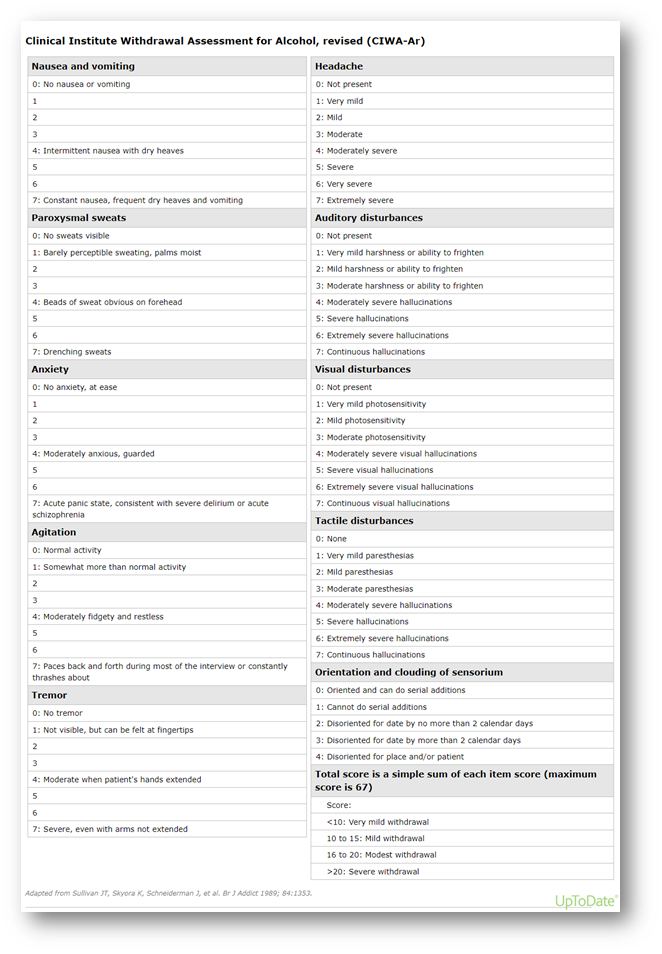
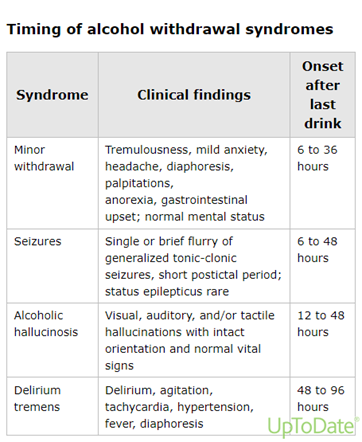
The CIWA protocol was created in the 1980s to help measure the severity of alcohol withdrawal symptoms and provide guided pharmaceutical treatment, which is based on a scored assessment scale of 10 diagnostic categories and is repeated with prescribed frequency. Asking a patient about their level of alcohol use in triage is particularly important in cases of tachycardia or agitation, because the onset of more serious withdrawal symptoms (especially seizures or delirium tremens) might be delayed until 48-96 hours after the patient’s last drink.
“It is critical to respect that alcohol withdrawal can be a life-threatening condition.”
Effective usage of the CIWA protocol can be complicated by hand-offs, level of care, intravenous (IV) medication protocols, and knowledge/experience with the assessment tool.
Although many factors influence any in-hospital mortality case, the hospital team considered this situation that was presented in the Safe Table to be possibly preventable. A multidisciplinary team undertook an RCA, which began by asking, “What should have happened?” The team then explored:
- Why the patient was not initially transferred from the emergency department (ED) to the intensive care unit (ICU)
- Why the CIWA score was so different from ED departure to the telemetry unit admission
- Why a subsequent transfer to ICU was delayed (or never occurred)
- Why the patient was under-medicated
The team’s analysis resulted in the following root cause statement:
The patient was not admitted or later transferred to the ICU BECAUSE specific guidelines (standard work) for defining the level of care required for patients withdrawing from alcohol did not exist.
The patient was still in the ED at the first physician’s change of shift, so the oncoming MD made the decision for admission, choosing the Telemetry Unit rather than ICU after discussion with the intensivist because the CIWA score (17, down from 19) didn’t warrant it, and there were no available beds in ICU. Upon arrival to the telemetry unit, the CIWA score was 24 and calls to the physician began and continued throughout the night as the score continued to rise with increasing symptomatology. Rapid Response Team nurses were also enlisted to help with assessment and management through the night. IV Ativan was given per protocol, but didn’t seem to be effective, as the CIWA score progressed to 28.
The need for IV Phenobarbital was determined and the hospitalist and pharmacist researched and conferred on the appropriate dosing (outside the critical care setting) for approximately four hours. The medication was finally given around noon. Two hours later the patient was wildly agitated and confused, had a large coffee ground emesis, and went into cardiac arrest. Intubation and extensive resuscitation did result in return of spontaneous circulation, but an emergency bronchoscopy revealed significant complications and the patient was maintained on comfort care only at the family’s request until his death shortly thereafter.
The RCA process evaluated the proximate causes (all the factors leading to the Root Cause Conclusion above) with “because” assertions that surfaced in the multidisciplinary discussion.
Proximate Cause Statements
- The hospitalist did not write transfer orders for the ICU because he conferred with the intensivist who instructed them to continue patient management on the floor and there was a misperception that the intensivist must “accept” the patient for transfer to the ICU.
- The hospitalist’s orders undermedicated patient symptoms because there were medication shortages at the time and there was no protocol for use of IV Phenobarbital versus IV Ativan outside of critical care.
- Nursing staff may not manage patients effectively because of unfamiliarity with the CIWA protocol and unease with administration of high doses of the required meds.
- The consulting pharmacist provided phenobarbital dosing recommendations that were determined to be inadequate to meet patient needs because they were based on external tertiary resources and there was no standardized treatment plan for phenobarbital use in the treatment of alcohol withdrawal.
Several specific actions were taken to address ALL the proximate causes and have been shared with all hospitals in the system in which this event occurred.
Actions Taken
- Pharmacy and critical care physicians partnered to establish a Phenobarbital Protocol for CIWA management, and the IV Medication List was amended to include the Phenobarbital protocol.
- Having discovered a lack of “standard work,” no existing protocol for usage of CIWA, and no education on scoring, nursing operations created a workgroup to address gaps in the CIWA policy and staff education. Multiple avenues for education and validation of understanding were implemented, highlighting that a score over 20 requires critical care.
- Physicians met to clarify key points for medical staff review and education related to when and how to escalate to a higher level of care. If an ICU bed is not immediately available, critical care resources will be brought to the bedside in the current unit.
These specific actions were shared with CHPSO members who attended Safe Table presentation. Contact CHPSO at info@chpso.org for more information. The CIWA scoring guideline is included below for reference.