Key Points:
- The Collaborative Healthcare Patient Safety Organization (CHPSO) has seen dramatic improvement in reducing unclassified events on its platform, dropping from 16.8% in 2022 to just 6.9% in 2024.
- Even when patients experience additional suffering, extended recovery, or psychological trauma, these impacts are frequently mislabeled as “no harm” if they do not result in catastrophic outcomes.
- Harm misclassification skews safety data and masks the true burden of harm.
Understanding Harm Misclassification
Harm misclassification occurs when hospitals downplay or incorrectly categorize patient safety events as “no harm” when actual harm has occurred. Though often underrecognized, harm misclassification significantly undermines accurate safety reporting and impedes meaningful improvement efforts.
Two important questions emerge: Why do health care organizations misclassify harm events? And what impact does this have on patient safety?
Key Findings from CHPSOData
To provide context to these questions, Figure 1 shows the volume of CHPSOData patient safety events from 2022-24 classified by patient harm level: No Harm, Harm, Unknown/Unclassified. Table 1 presents the percentages of these patient safety events by harm level.
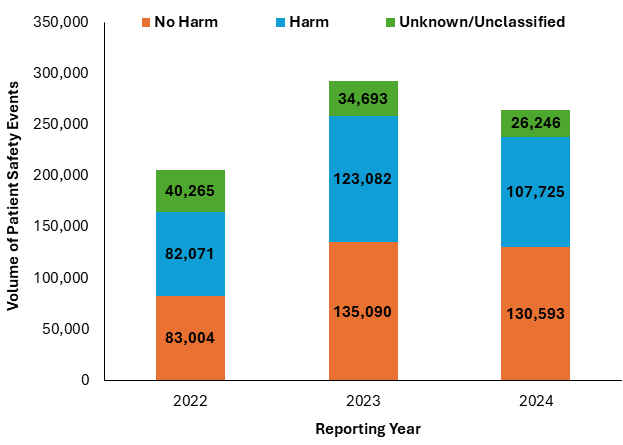
Figure 1 shows overall event volume growth: The number of reported events increased significantly from 2022 to 2023, then slightly decreased in 2024 (though this probably represents incomplete reporting for 2024).

Table 1 highlights several key patterns in event classification:
- Increase in the “No Harm” Classification: There’s an upward trend in “No Harm” events from 40.4% in 2022 to 49.4% in 2024 — a 9 percentage point increase. This significant shift warrants attention — is it due to improved safety practices or changing classification tendencies?
- Consistent “Mild Harm” Patterns: “Mild Harm” classifications remain remarkably stable around 27% to 28% across all three years, suggesting consistent identification of these less severe events.
- “Moderate Harm” Fluctuation: “Moderate Harm” events show some variability (10.9% to 13.0% back to 11.3%). This could reflect changes in reporting practices, or it may be due to changes in actual safety performance.
- Low Serious Safety Events: Severe harm and death consistently represent approximately 1.4% to 1.7% of all events combined, showing minimal change over the reporting period.
- Improved Classification Compliance: The most dramatic improvement is in unclassified events, dropping from 16.8% in 2022 to just 6.9% in 2024, indicating substantially better reporting discipline or improved data quality capture within CHPSOData.
Contributing Factors
Many factors contribute to harm misclassification, ranging from variability in classification schemas to fear of repercussions and lack of basic understanding of harm scales. Accurate assessment is further complicated by:
- Outcome Bias: The tendency to judge decisions based on their outcomes rather than the quality of the decision-making process
- Retrospective Minimization: The tendency to downplay the seriousness of events after they have occurred, especially when no catastrophic outcome resulted
- Normalization of Deviations: The process by which deviations from standard practice become accepted as normal over time
Assessment Inconsistencies
Harm assessment by health care professionals — primarily nurses, who make up the largest percentage — has been found inconsistent both among peers and even by the same individual. Theoretically, harm classifications should align with objective criteria; in practice, however, misperceptions can result in subjective assessments.
Common Scenarios of Misclassification
The following themes identified within CHPSOData show consistent patterns of harm misclassification:
- Delays in care are often classified as “No Harm” if the patient eventually received proper treatment, but intermediate suffering and extended recovery are ignored.
- Medication errors are frequently labeled “No Harm” when they do not produce catastrophic outcomes, even when patients experience side effects or require additional monitoring.
- Procedural complications that require additional interventions but are ultimately resolved are often labeled “No Harm,” despite the patient experiencing pain or extended hospitalization.
- Psychological harm is almost universally underreported and misclassified, despite significant impact on patients’ well-being and trust in health care.
Consequences of Harm Misclassification
The primary impact of misclassification is a false sense of safety, and the secondary impact is that it undercuts safety initiatives. Additionally, it hinders root cause analysis for events that result in substantial harm, which can lead to recurring issues and ineffective solutions. Misclassification also diminishes organizational learning opportunities and fails to acknowledge patient experiences.
Improvement Strategies
Several strategies can be implemented to improve harm classification and patient safety reporting:
- Education and Training: Provide comprehensive programs to increase understanding of harm scales and classification criteria.
- Standardized Assessment Tools: Implement consistent frameworks for evaluating harm across all departments and facilities.
- Just Culture: Foster an environment where accurate reporting is valued over favorable statistics.
- Patient Perspective: Incorporate patient experiences into harm assessment processes.
- Regular Classification Audits: Review classification practices to identify and address systematic biases.
By addressing harm misclassification and promoting accurate assessment, health care organizations can better understand the true impact of safety events and develop more effective strategies toward harm prevention.
Contact Vivian Eusebio, patient safety clinical advisor, at veusebio@chpso.org with questions or comments.

