Introduction
The COVID-19 pandemic caused myriad adverse health conditions, both physical and mental. The physical effects of the virus included a range of symptoms including, but not limited to fever, cough, shortness of breath, and loss of taste or smell (Centers for Disease Control and Prevention, 2022).
In terms of mental health, isolation proved to be a serious issue for the population’s overall mental health. Humans by nature are social beings, relationships and interactions with others are not only beneficial, but necessary. The pandemic resulted in long periods of quarantine for individuals — depriving them of much-needed social interaction. During the pandemic, it was found that there was a significant increase in feelings of loneliness, depression, and anxiety in the general population (Ramos, 2022).
Due to this spike in the decline of mental health during the epsilon variant, there is reason to investigate the impact on people without pre-existing mental disorders and the degree of impact of those with pre-existing or diagnosed mental disorders. This report shows the changes of the prevalence of four mental disorders (depressive disorder, bipolar disorder, schizophrenia disorder, depressive episode) among California hospital discharges before and after the epsilon COVID-19 variant surge.
Method
Complete 2018-21 discharge data are from 71 California hospitals that reported to HQI’s Hospital Quality Improvement Platform. To calculate the rates presented below, ICD codes F33, F31, F20, and F32 were used to identify patients with a primary diagnosis for the four mental disorders: depressive disorder, bipolar disorder, schizophrenia disorder, and depressive episode. Monthly prevalence rates were calculated by summing the number of discharges for each disorder per month, and then dividing the total number of discharges for the month. To provide context, the time series plot also shows the statewide monthly number of new COVID-19 infections from the CHHS Open Data Portal.
Results
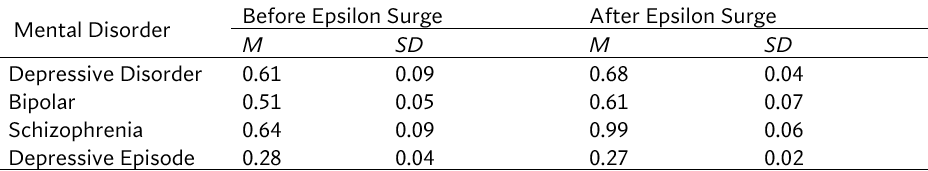
Figure 1 shows the monthly percentage of discharges in the sample of California hospitals from 2018-21 for the four mental disorders (depressive disorder, bipolar disorder, schizophrenia disorder, depressive episode). Also shown in the chart for reference purposes, is a black line that represents incidents of COVID-19 cases from 2020-21. Looking at the chart, it appears all four disorders subsequently increased following the peak in cases from the winter 2020 to the beginning of 2021. The increase in lag of disorders is greater than people simply waiting for care as demonstrated in Table 1.

Time Series Analyses of Prevalence for Four Mental Disorders Among Inpatient Discharges Following with the Epsilon COVID-19 Variant Surge
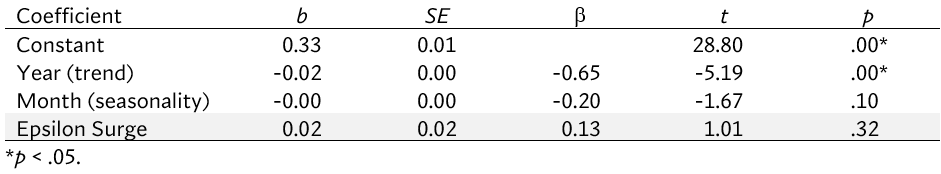
To quantify the impact of the epsilon surge on inpatient mental disorder encounters, a series of four time-series analyses, one for each diagnoses, was conducted. In each time series analysis, the effect of linear trend was adjusted using a parameter that consisted of serially increasing values as a function of the calendar year. For example, 2019=0, 2020=1, etc. In addition, to adjust for seasonality, a variable representing month and year ranging from 1-12, where 1=January and 12=December was used in a model. The intervention parameter for the effect of epsilon was estimated using an indicator variable consisting of 1’s from February to May, and 0’s elsewhere. Hence, the regression parameter for the epsilon effect represents the percentage point change increase in the inpatient admission rate per 100,000 discharges for the mental disorder analyzed. The results of the time series analyses are presented in the following sections.
Depressive Disorder
The overall time series model for depressive disorders was statistically significant and accounted for 56.4% of the variability of the depressive disorder discharge rate, F(3,44) = 18.98, p < .05. Specifically, the epsilon surge from winter 2020 to spring 2021 was associated with a significant 0.18 percentage-point increase in depressive disorder discharges, which corresponds to a 29.5% increase from the pre-epsilon surge level.

Bipolar Disorder
Based on the results, the epsilon surge from winter 2020 to spring 2021 was associated with a significant 0.12 percentage-point increase in bipolar disorder discharges (23.9% increase from pre-epsilon level). The overall linear time series model for bipolar disorder was statistically significant and accounted for 29.6% of the variability of the bipolar disorder discharge rate, F(3,44) = 6.16, p < .05.

Schizophrenia Disorder
The findings showed that during the epsilon surge from winter 2020 to spring 2021, there was a significant 0.28 percentage-point increase in schizophrenia disorder discharges (43.6% increase from pre-epsilon level). The overall linear time series model for schizophrenia disorder was statistically significant and accounted for 63.0% of the variability of the schizophrenia disorder discharge rate, F(3,44) = 25.00, p < .05.

Depressive Episode
It was shown that the overall linear time series model for depressive episode was statistically significant and accounted for 42.7% of the variability of the depressive episode discharge rate, F(3,44) = 10.92, p < .05. However, the epsilon surge from winter 2020 to spring 2021 was not associated with a significant percentage-point change in depressive episode discharges from the pre-epsilon surge level.
Discussion
It was found that the epsilon surge was associated with a significant increase in three of the four mental disorders discussed, namely schizophrenia disorder, depressive disorder, and bipolar disorder. The most significant finding from the research was that there was a lag in the increase of patient admissions for these disorders following the epsilon surge. This was shown in three of the four most prevalent diagnoses (schizophrenia disorder, depressive disorder, and bipolar disorder). According to Spudich and Nath (2022), there may be significant neurological effects of contracting COVID-19, including psychosis and depression. Both features are prevalent in schizophrenia and the other disorders that increased. It was found that individuals have been experiencing effects of what is called “Long COVID,” meaning they have lingering symptoms. This could be a potential reason for the lagged increase found for three of the disorders.
The mental disorder found to have the greatest increase was schizophrenia. There may have been a larger increase in patient discharges with this diagnosis because of the dramatic features of the diagnosis. The symptoms associated with this diagnosis must include two or more of the following symptoms: delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative symptoms (i.e., the reduction of an action rather than morally speaking) (American Mental Association, 2014). Another possibility for the dramatic peak in schizophrenia diagnoses is that COVID-19 triggered symptoms in individuals.
It is also interesting to note that three of the four most-prevalent diagnoses share a depressive component. Depressive episode and depressive disorder are both entirely defined by depressive features, and bipolar disorder is defined by fluctuating between depressive episodes and manic episodes (American Mental Association, 2014). A depression diagnosis requires the individual to experience five or more symptoms including, but not limited, to depressed mood most of the day, diminished interest in most activities, insomnia, fatigue, and feelings of worthlessness for at least a two-week period (American Mental Association, 2014). It is possible that depression was prevalent because of the impact that social isolation had on individuals. Many individuals experienced the symptoms associated with a depressive diagnosis, so this may explain why there was an increase in associated diagnoses. However, each of the four diagnoses follows the pattern of lagged increases following the peak in COVID-19 cases in the winter 2020, so the results suggest that COVID-19 may have indeed impacted the prevalence of disorders with a depressive component.
The study results suggest lagged increases in the prevalence of these disorders corresponding with the epsilon surge of the pandemic. The reasons that the increases lagged the actual COVID-19 surge warrant further exploration. The research being conducted on the effects of “Long COVID” should be continued, especially its impact on mental health. It is important to understand how and why there was a lag in the association between the epsilon variant and mental health diagnoses to be able to protect persons with mental health diagnoses such as schizophrenia disorder, bipolar disorder, depressive disorder, and depressive episode during future pandemics.
References
American Mental Association. (2014). Diagnostic and Statistical Manual of Mental Disorders, DSM-5. American Mental Association.
Centers for Disease Control and Prevention. (2022, March 22). Symptoms of COVID-19.
Ramos, K. (2022). Mental Health Impacts of the COVID-19 Pandemic. Generations, 46(1), 1–8.
Spudich, S., & Nath, A. (2022). Nervous system consequences of COVID-19. Science, 375(6578), 267-269.
