Key Takeaways
- 80% of SEP-1/2 and SEP-3 cases overlap
- COVID-19 caused both SEP-1/2 and SEP-3 case mortality rates to increase
- SEP-3 has a much higher case mortality rate (10.1%-15.6%) than SEP-1/2 only (0.6%)
Introduction
Sepsis is a serious medical condition that can be life-threatening and devastating to those afflicted. It is defined as the catastrophic response when the body cannot fight off a systemic infection (septicemia), potentially leading to organ failure and death.1 Septicemia is fundamentally another term for sepsis, which is when an infected person’s blood is poisoned by toxins due to the body’s inability to fight an infection. The infection causal agents may range from bacterial to viral to parasitic. In 2022, 51.1% of all inpatient deaths in California hospitals involved sepsis.
Case Definitions for Sepsis
Sepsis is diagnosed by medical professionals, and the diagnostic criteria have changed over time. Many people may not realize that the term “sepsis” is underpinned by three International Consensus Definitions (1991: Sepsis-12, 2001: Sepsis- 23, and 2016: Sepsis 34). Essentially, however, the diagnostic criteria for SEP-2 were very similar to those of SEP-1, so they are typically combined (SEP-1/2). In 2016, the third international consensus definitions for sepsis and septic shock (SEP-3) were released, which defines sepsis as the presence of both septicemia and one or more organ dysfunctions.
Proxy Definitions for Sepsis for Research
For purposes of conducting research, conditions such as sepsis are proxy identified through the presence of diagnosis codes, or combinations of such codes, on patient records. SEP-1/2 can be identified in encounter data through the presence of diagnosis codes for septicemia5. However, SEP-3 involves the use of codes for septicemia as well as those for organ dysfunction. Both must be present to meet the proxy case definition of SEP-3. Given that organ dysfunction can lead to total organ failure and death, SEP-3 is focused on cases of sepsis that are more severe than cases of SEP-1/2. The algorithm that the Hospital Quality Institute (HQI) follows to calculate SEP-3 is available here and the codes for SEP-3 and SEP-1/2 are available here. Note that of the 69 septicemia codes that are part of the SEP-3 case definition, 27 (39%) are included in the SEP-1/2 case definition. The remaining 42 (61%) septicemia codes that are part of the SEP-3 case definition are unique to SEP-3 and include newer codes that have been added since the SEP-1/2 codes were introduced.
SEP-1/2 and SEP-3 Incidence Rates
Figure 1 shows the percentage of inpatient discharges meeting the SEP-1/2 only, SEP-3 only, or both SEP-1/2 and SEP-3 proxy case definitions in California hospitals during 2022.
From Figure 1, we can see that:
- About 80% of cases met both the SEP-1/2 and SEP-3 proxy definitions
- Roughly 20% of cases meeting the SEP-1/2 definition did not also meet the SEP-3 definition (no organ dysfunction was noted)
- SEP-3-only, which reflects the usage of newer septicemia codes that are unique to SEP-3, is identified as being the lowest diagnostic rate, while SEP-1/2-only is more common.

SEP-1/2 and SEP-3 In-Hospital Case Mortality Rates
Figure 2 shows the in-hospital case mortality rates of inpatient discharges meeting the SEP-1/2 only, SEP-3 only, or both SEP-1/2 and SEP-3 proxy case definitions in California hospitals during 2022.
From Figure 2, we can see that:
- Cases that met both the SEP-1/2 and SEP-3 case definitions had the highest mortality rate (15.6%), which make sense given that these cases were all experiencing organ dysfunction
- On the other hand, cases that met only the SEP-1/2 definition had the lowest mortality rate (0.6%)
- SEP-3-only cases, although a small ‘slice in the pie’ of actual inpatient sepsis cases, nonetheless has a devasting case mortality rate (10.1%)
- Since SEP-3 includes organ dysfunction as well as septicemia in its proxy definition and code set, it is not surprising that SEP-3 overall tends to have a higher case mortality rate than SEP-1/2

SEP-1/2 Historical Incidence and Case Mortality
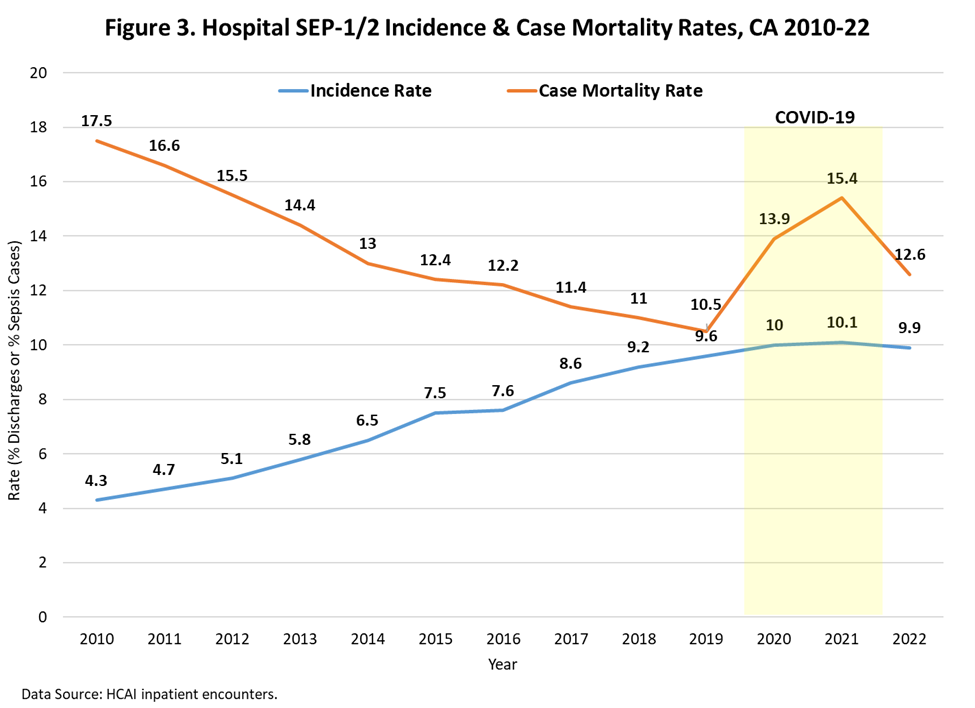
Figure 3 shows the in-hospital SEP-1/2 incidence and case mortality rates of inpatient discharges meeting the SEP-1/2 proxy case definition in California hospitals from 2010-2022.
From Figure 3, we can see that:
- Prior to COVID-19, the SEP-1/2 incidence rate increased from 4.3% to 9.6% of all inpatient encounters
- At the same time, the SEP-1/2 case mortality rate decreased from 17.5% to 10.5%
- The COVID-19 epidemic was associated with a drastic increase in SEP-1/2 case mortality rates, causing them to spike and peak at 15.4% in 2021
- Case-mortality remained higher than expected after COVID at 12.6% in 2022
- The COVID-19 epidemic was associated with a reduction in the year-over-year increasing trend in SEP-1/2 incidence
SEP-3 Historical Incidence and Case Mortality
Figure 4 shows the in-hospital SEP-3 incidence and case mortality rates of inpatient discharges meeting the SEP-3 proxy case definition in California hospitals from 2010-2022.
From Figure 4, we can see that:
- Compared to SEP-1/2, the SEP-3 incidence rate is lower, but the case mortality rate is higher
- Prior to COVID-19, the SEP-3 incidence rate increased from 2.9% to 7.3% of all inpatient encounters
- At the same time, the SEP-3 case mortality rate decreased from 24.2% to 13.5%
- The COVID-19 epidemic was also associated with a drastic increase in SEP-3 case mortality rates, causing them to spike and peak at 18.9% in 2021
- Case-mortality remained higher than expected after COVID at 15.6% in 2022
- The COVID-19 epidemic was associated with an initial increase in the year-over-year increasing trend in SEP-3 incidence, followed by a reduction from expectation

Correlations among SEP-1/2 and SEP-3 Incidence and Case Mortality
Figure 5 shows a heatmap illustrating the correlations among SEP-1/2 and SEP-3 incidence and case mortality rates.
From the heatmap, we can see that:
- The incidence rates of SEP-1/2 and SEP-3 are strongly correlated (r = 0.98)
- The case mortality rates of SEP-1/2 and SEP-3 are also strongly correlated (r = 0.95)
- The correlation between incidence and death is similar for SEP-3 (r = 0.45) and SEP-1/2 (r = 0.47)

Conclusions
- Most SEP-1/2 cases are also SEP-3 cases; however, all SEP-3 cases are not necessarily cases of SEP-1/2; the overlap is roughly 80%
- SEP-3 incidence is lower than SEP-1/2, but the SEP-3 case mortality rate is higher; this suggests SEP-3 cases are more closely tied to fatality rates
- Prior to COVID-19, it appears that as the SEP-3 incidence rate increased, most likely due to earlier identification, the SEP-3 case fatality rate decreased
- COVID-19 had a drastic impact on the SEP-1/2 and SEP-3 case fatality rates, causing them to increase, and remain elevated
1 https://www.cdc.gov/sepsis/about/?CDC_AAref_Val=https://www.cdc.gov/sepsis/what-is-sepsis.html
2 Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM consensus conference committee. American college of chest physicians/society of critical care medicine. Chest 1992;101:1644–55. doi: 10.1378/chest.101.6.1644.
3 Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med 2003;29:530–8. doi: 10.1007/s00134-003-1662-x.
4 Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016;315:801–10. doi: 10.1001/jama.2016.0287
5 Section 2.1 – Severe Sepsis and Septic Shock (SEP), specifically see Table A.1 .
