A “near miss” in health care is when an error or adverse event is narrowly avoided. Though often underreported and underrecognized, near misses are significant indicators of potential patient safety hazards. While exact statistics vary due to reporting practices and definitions, studies suggest that near misses are relatively common occurrences. So, here’s the million-dollar question: Why do health care organizations underreport these near occurrences, which could result in learnings that prevent patient harm?
To provide context:
- For every adverse event that occurs, there were between three and 300 near misses. (British Medical Journal)
- Medical errors, including near misses, contribute to tens of thousands of deaths each year in the United States alone. (Institute of Medicine)
- A 2022 study conducted in a single Swedish hospital concluded that “incident reporting and daily safety briefings identified 7.8 and 31.9 near-misses per 1,000 patient-days, respectively.” (Journal of Patient Safety)
- During the 2023 Agency for Healthcare Research and Quality conference, data were presented that suggested near-miss events should comprise approximately 44% of the total safety reports within an organization.
Many safety reporting systems rely on voluntary submissions, so these statistics likely underestimate the true prevalence of near misses during routine operations. The decline in submissions is further exacerbated during heightened demand, such as the pandemic years. These findings were disclosed by CHPSO in its 2021 examination of COVID-19, which highlighted the impact on staffing shortages.
To investigate the frequency of near-miss events in CHPSOData, the table below illustrates the distribution of this event report type in 2022, compared to incidents and unsafe conditions. Additionally, it shows how these event report types (e.g., incident, near-miss, unsafe condition) are distributed among the most prevalent event categories identified based on CHPSO’s enhanced event classification taxonomy.
Table 1. Distribution of Event Report Types for the 10 Most Prevalent Event Categories in CHPSOData Based on the Enhanced Event Classification Taxonomy Using “Top 1” Methodology, 2022
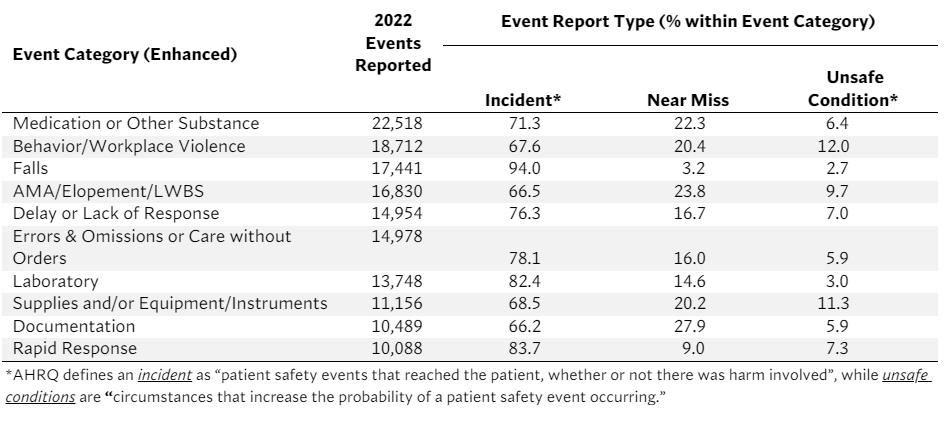
Predictably, medication errors emerged as the most frequently reported event category. Nevertheless, only 22.3% of the medication errors were near-miss event types, while 71.3% were incidents — highlighting a nearly 50-point gap. This trend exists across all event categories, with “falls” having the lowest reported near-miss percentage of 3.2%. Notably, “documentation” exhibited the highest percentage of near-misses at 27.9%, confirming what many organizations identify as a commonly reported near-miss event.
It’s important to note that since CHPSOData’s launch in October 2022, only 11% of all events reported are near misses, while 19% of events are “uncategorized” without an assigned event report type. Furthermore, 45% of all facilities with events in CHPSOData have never reported a near-miss event.
So, what do these data points tell us about reporting near-miss events?
Many would acknowledge that near-miss reporting differs among health care organizations. Nevertheless, the analysis of 2022 data reveals many health care entities do not report or underreport near-miss events. This trend isn’t confined solely to CHPSO members.
Well-documented factors contribute to underreporting of near-miss events or the lack of report submissions. The primary factor is that CHPSOData is a voluntary reporting system. As a result, mandatory fields or requirements for reporting are absent. Secondly, fear of blame or retribution can result in health care staff being hesitant to report near-miss events. Thirdly, underreporting may result from a lack of awareness of what constitutes a near miss or a failure to understand its importance. Lastly, time constraints can make it difficult to properly report near misses. While there are other contributing factors, these are the most common.
Several strategies can be implemented to improve data submissions and enhance near-miss reporting:
- Education and training: Provide comprehensive education and training programs to health care staff to increase awareness of near misses and the importance of reporting them.
- Streamlined reporting processes: Simplify and streamline reporting systems to make it easier and more efficient for staff to report near misses.
- Just culture: Foster a culture of trust, transparency, and learning where staff feel comfortable reporting near misses without fear of blame or retaliation.
- Feedback and follow-up: Provide timely feedback to staff who report near misses and ensure that corrective actions are taken to address underlying issues.
- Leadership support: Engaging organizational leaders in promoting near-miss reporting initiatives and allocating resources to support these efforts.
By addressing barriers to reporting and promoting a culture of safety and learning, health care organizations can improve near-miss reporting and — most importantly — improve patient safety outcomes.
