
Enrollment in the Hospital Quality Improvement Platform (HQIP) jumped substantially in the last quarter due to increased registration among hospitals participating in L.A. Care Health Plan’s Hospital Pay-for-Performance (P4P) incentive program. Recent updates to HQIP include a new report on 30-day Hospital-Wide All-Cause Unplanned Readmission that is more closely based on Centers for Medicare & Medicaid Services (CMS) methodology.
HQIP is a secure, web-based platform that provides quality measures for conditions most affected by hospital quality initiatives. Through the platform, hospitals gain access to clinically rich, timely reports to help easily identify opportunities for improvement and areas for focus. It is free to all California Hospital Association members, does not connect to hospitals’ electronic health records system, and uses data hospitals already report to the California Department of Health Care Access and Information (HCAI), the National Healthcare Safety Network (NHSN), and the California Maternal Quality Care Collaborative.
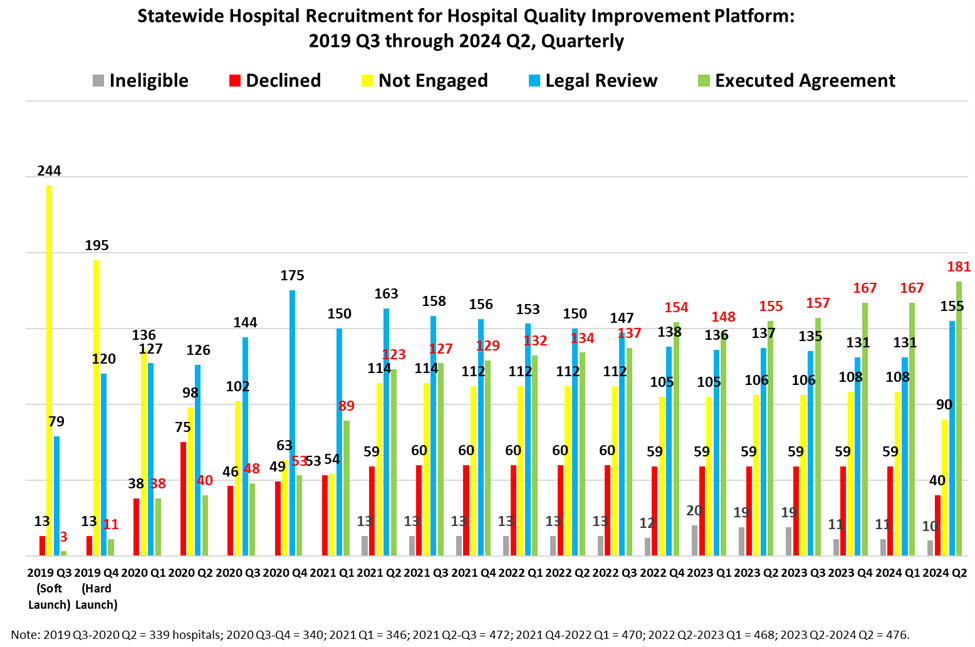
Since launching in October 2019:
- 333 of 476 hospitals have seen a demo of the platform
- 181 hospitals have executed agreements
- 155 hospitals have participation agreements under legal review
NEW FEATURES AND UPDATES
In addition to participation expansion, here’s what’s new to HQIP since the last update:
- HQI held its second HQIP Quarterly User Group Meeting on May 23. The next meeting is scheduled for Aug. 22 from 10 to 11 a.m. (PT)
- Continued refinements to the integrated SpeedTrack Analytics reports to help hospitals meet the annual HCAI Hospital Equity Reporting requirements that start in September 2025
- A mock local health plan report for 2024 Hospital P4P Program for L.A. Care Health Plan
- New 30-day Hospital-Wide All-Cause Unplanned Readmission (HWR) report based on the CMS methodology. The old readmission report currently in the system will be removed in 2025
- Minor modifications to the “ED Encounter Types” filter
With feedback about features or measures, email HQIAnalytics@hqinstitute.org.
WHAT’S NEXT
- HQI is still developing a Sepsis 1-2-3 report presenting incidence and mortality for multiple sepsis definitions, along with readmissions and missed sepsis opportunities
- Condition-specific and procedure-specific readmission reports are in development based on the CMS methodology
- Automated reports are planned for later this year to streamline the production of local health plan reports on data uploads and measure outcomes across network hospitals
- Recruitment of L.A. Care Health Plan hospitals is ongoing
- A new emergency department (ED) report presenting the incidence rates of ED encounters (including those admitted as Inpatient) by Clinical Classifications Software Refined (CCSR) Diagnosis Chapters and CCSR Clinical domains developed by AHRQ
- Also in development is a new report that will present the incidence of Ambulatory Surgery encounters grouped by the Centers for Disease Control and Prevention’s (CDC) NHSN Surgical Site Infection Events Operative Procedure Code Mappings (ICD-10-PCS and CPT)
ABOUT THE PLATFORM
Features include:
- Access to hospital performance data from various sources, integrated into a centralized platform
- Tools to understand your hospital’s quality performance and compare standardized measures to statewide benchmarks and peers
- The ability to explore same-year quality performance for your hospital, rather than waiting up to 20 months for statewide files to be released
- An intuitive interface that provides a window into inpatient and emergency quality indicators
- Secure data within HIPAA-qualified encrypted data systems
Quality measures include:
- Inpatient case mix demographics, comorbidities, index
- ED discharge analytics (comorbidities, volume, demographics, revisits)
- Ambulatory surgery demographics
- Agency for Healthcare Research and Quality patient safety indicators
- Sepsis incidence and mortality
- Maternity measures
- Discharge volume by source (inpatient, ED, ambulatory surgery)
- Social determinants of health
- Chronic physical and behavioral conditions
- NHSN measures, trends, and details
There are many options for benchmarking your hospital’s performance:
- All CHA member hospitals
- Other critical access hospitals
- Other rural hospitals
- Other children’s hospitals
- Other teaching hospitals
- Other hospitals with the same payer (e.g., IEHP, PHC)
- Your hospital’s past performance
- Other CHA member hospitals:
- In the same health system
- In the same general region
- In the same health service area
- In the same metropolitan statistical area
- With similar bed size
- With the same type of control (e.g., non-profit)
- With the same license type
- With similar Medicare payer mix
- With similar Medi-Cal payer mix
- With the same adult/children’s trauma level designation
- With similar inpatient discharge volume
- With same ED service level (e.g., basic, standby)
- With similar outpatient visit volume
For hospitals interested in participating, all it takes are three easy steps:
- Execute the cost-free HQI-Hospital Service Agreement and HQI-Hospital Business Associated Agreement.
- Follow the HCAI Patient-Level Administrative Data (SIERA) HQIP Upload Instructions to securely submit copies of recent HCAI Patient-Level Administrative Data for ED, ambulatory surgery, and inpatient encounters.
- Follow our NHSN HQIP Group Join Instructions to confer rights to HQI’s NHSN group on the CDC’s Secure Access Management Services web portal.
For more information about the HQIP or to schedule a 30-minute demo, visit the HQI website or email HQIAnalytics@HQInstitute.org.

